What we know - and we don’t know about the virus, known as SARS-CoV-2 (COVID-19)
Saanvi Sharma1*, Jyoti Bhardwaj2*
1Pennbrook Middle School, North Wales, PA, USA, 2Acton-Boxborough Regional High School, Acton, MA, USA
* Both authors contributed equally
***The article used information that was made public on May 21, 2020. Due to the rapidly developing situation surrounding Covid-19, some information may be out of date.***
The recent SARS-CoV-2 outbreak began in the city of Wuhan (Hubei, China) in December 2019 (4). It soon spread in the city and infected thousands of people leading to a broader health problem that resulted in the death of about 500,000 people. On March 11, 2020, the World Health Organization (WHO) named COVID-19, a pandemic. As of June 26, 2020, COVID-19 has spread to 213 countries, and the current number of confirmed COVID-19 cases stands at 9,906,585 with 496,915 deaths(1). Europe and the USA were the epicenter of this pandemic initially which has now changed to Brazil and Russia as the cases are rising every minute due to the increased availability of testing facilities.
What are coronaviruses?
Coronaviruses (CoV) are positive-sense, single strand enveloped large RNA viruses belonging to the family coronaviridae. The name coronavirus is derived from the Latin corona, meaning crown, because under electron microscopy the bulbar projections by the viral spike (S) peplomers appear crown-like in shape (Fig1). These viruses generally cause severe upper respiratory tract infections in humans and can also commonly infect birds and mammals, causing gastroenteritis and respiratory infections. Currently, there are three types of CoV that can severely infect humans: middle east respiratory syndrome (MERS-CoV), severe acute respiratory syndrome (SARS-CoV), and SARS-CoV-2. There are four other types of coronaviruses that only cause some mild symptoms, such as the common cold. These viral strains have all developed and mutated from a virus that originated in animals (8). The most recent outbreak of coronavirus disease, COVID-19, is an infection caused by the recently identified virus, SARS-CoV-2
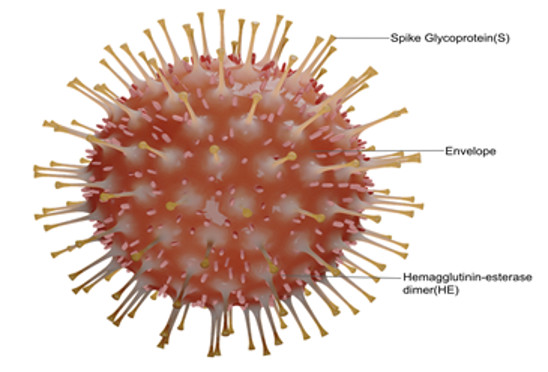
Figure 1: SARS-CoV-2 virus has a crown-like appearance due to small bulbar projections formed by the spike proteins.
SARS-CoV-2 is made up of four structural proteins and an RNA strand, which stores its genetic information. Once the virus passes through the mouth, nose, or eyes, it attaches to a protein known as ACE2 (angiotensin converting enzyme 2) expressed on the surface of respiratory tract cells, allowing the virus to enter the cells(10). This results in some of the symptoms related to the novel coronavirus. Furthermore, as the virus attaches to the cell, the RNA (ribonucleic acid) is released; thus, causing the infected cell to create proteins according to the RNA instructions (13). RNA, in basic terms, is the instructions that the cell uses to make proteins. Each infected cell can create about one million copies of the virus before being degraded. The massive copying of the virus relates to its ability to spread rapidly and infect other cells within the respiratory system.
What are the symptoms of COVID-19?
The SARS-CoV-2 virus is an RNA virus that primarily affects the respiratory system. RNA viruses spread by attaching to a host cell inside the body. Once inside the cell, the virus will release its RNA, altering the cell’s DNA and forcing the cell to duplicate the virus (13). The incubation time of this virus ranges from 2-14 days with a mean period of 5 days. Although a majority of the patients infected with COVID-19 generally develop mild to moderate symptoms and recover without requiring hospitalization, people with underlying medical conditions (diabetes mellitus, chronic lung disease, and cardiovascular disease) and those over 60 years old have a higher risk of developing severe disease and death. Common symptoms include fever, tiredness, shortness of breath, and dry cough. However, some patients infected with the virus have also reported aches and pains and sore throats. A small minority of patients have reported diarrhea, nausea or a runny nose. COVID-19 has proven to have a high transmissibility rate, which has led to spikes in the number of patients who have tested positive for the virus (14).
How is it different from other viruses?
Although SARS-CoV-2 is believed to act like other coronaviruses, there are key differences between them. First, most of the known coronaviruses only cause mild diseases and result in a common cold. The two other known coronaviruses SARS-CoV-1 and MERS-CoV, which cause SARS and MERS respectively, are more severe and have higher death rates than the milder strains of coronaviruses (9). However, COVID-19 is even more severe than SARS and MERS and has resulted in more deaths. Furthermore, COVID-19 has a higher infection rate compared to SARS and MERS.
Although COVID-19 has shown to cause flu-like symptoms, it should not be treated like the flu. For starters, there is not much known about how SARS-CoV-2 is able to transmit so rapidly between humans and how long it can survive on different kinds of surfaces. Moreover, the mortality rates are much higher with this virus (0.6 -11 %) compared to that of the seasonal flu (0.1%). Next, the common flu is not a pandemic; it is only considered to be an epidemic, which means that unlike COVID-19, it has not spread as rapidly throughout the world. Finally, due to the vast knowledge that scientists have about the flu, a vaccine for it is available for people to take each year. However, there is no vaccine for SARS-CoV-2.
Why has COVID-19 been so successful in infecting humans?
This novel virus primarily spreads through person-to-person contact. Similar to the common cold, COVID-19 spreads through droplets created when a person sneezes or coughs. When a person who has become infected with the virus coughs or sneezes, people in close contact with them could inhale the contaminated droplets into their lungs and subsequently contract the virus (2). However, some people who become infected with the virus may not develop symptoms of the disease and are known as asymptomatic carriers. These asymptomatic carriers can end up spreading the virus without even knowing it. Therefore, to avoid spreading the virus unknowingly from person to person, it is essential to wear a face mask. In addition to person-to-person spread, COVID-19 can also spread by touching contaminated surfaces. Touching a surface contaminated with SARS-CoV-2 droplets and then subsequently touching their nose or mouth would cause a person to introduce the virus to their respiratory tract and could cause them to contract COVID-19. Thus, people need to wash their hands frequently and wipe down surfaces that could potentially be contaminated with SARS-CoV-2. Although contracting the virus from a surface does not occur frequently, there are specific surfaces people should avoid. For example, SARS-CoV-2 can stay within the air for about three hours and has been reported to remain on surfaces made of steel and plastic for up to three days.
Are there any treatment options against COVID-19?
There is no treatment currently available for the COVID-19. Both the CDC and the WHO have recommended several preventative measures that people can take to prevent the spread of the virus, such as wearing a mask. People can also help prevent its spread by maintaining good personal hygiene and avoiding close contact with others who might be sick or are at risk for contracting the virus. Social distancing has also been implemented in many parts of the world to mitigate the spread of COVID-19. In the meantime, scientists are currently working on potential vaccines for SARS-CoV-2 and are hoping to have one ready by early 2021 if everything goes with the plan. Scientists across the world are also testing potential drugs to target the virus. Very recently, the USFDA approved remdisivir (an antiviral drug previously tested in the fight against Ebola virus) for the treatment of severe COVID-19 patients. This drug has been shown to reduce the time of hospital stay and recovery by 4 days. Another drug that is currently being tested is chloroquine. Although chloroquine has traditionally been prescribed for malaria, lupus, and rheumatoid arthritis, it showed some promising effects on the SARS-CoV-1 outbreak in 2002 by hindering the virus’s ability to replicate in human cells. Due to its similarities with SARS-CoV-1, SARS-CoV-2 may be affected similarly by this drug. Currently, clinical trials are being conducted to test chloroquine under USFDA directives. In many places, a combination of HIV drugs is being tested to impede the growth of the virus. However, these combinations have not shown any promising results thus far. Furthermore, steroids were used to reduce the death rate of patients with severe Covid-19 (11). Larger patient testing using randomized clinical trials is required to fully establish the validity of these repurposed drugs for COVID-19.
Questions that we do not have answers to yet
- Where did SARS-CoV2 originate from?
- Will the virus spread at a slower rate during the summer?
- Why do some people have severe symptoms of this virus, while others are asymptomatic?
- Will SARS-Cov2 mutate?
- How does our immune system react to CoV-2?
- Will there be a second wave of COVID-19?
- What vaccines under trial will efficiently prevent the spread of the virus in the future?
For More Information:
- The Lancet COVID-19 Resource Centre; http://www.thelancet.com/coronavirus
- Centers for Disease Control; http://www.cdc.gov/coronavirus/
- The New England Journal of Medicine; http://www.nejm.org/coronavirus
- World Health Organization; http://www.who.int/emergencies/diseases/novel-coronavirus-2019
- National Institute of Health; http://www.nih.gov/health-information/coronavirus
References
1. ArcGIS Dashboards, gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6.
2. Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, www.cdc.gov/coronavirus/2019-ncov/about/.
3. Backer, Jantien A, et al. “Incubation Period of 2019 Novel Coronavirus (2019-NCoV) Infections among Travellers from Wuhan, China, 20–28 January 2020.” Eurosurveillance, vol. 25, no. 5, 2020, doi:10.2807/1560-7917.es.2020.25.5.2000062.
4. “COVID-19 Coronavirus Epidemic Has a Natural Origin.” ScienceDaily, ScienceDaily, 17 Mar. 2020, www.sciencedaily.com/releases/2020/03/200317175442.htm.
5. Cheng, Hao-Yuan. “Contact Tracing Assessment of COVID-19 Transmission Dynamics in Taiwan.” JAMA Internal Medicine, 1 May 2020, jamanetwork.com/journals/jamainternalmedicine/fullarticle/2765641.
6. “Coronavirus Cases:” Worldometer, www.worldometers.info/coronavirus/.
7. Gallagher, James. “Coronavirus: What We Still Don't Know about Covid-19.” BBC News, BBC, 29 Mar. 2020, www.bbc.com/news/health-52006988.
8. Hauck, Grace. “The Basics on the Coronavirus: What You Need to Know as the US Becomes the New Epicenter of COVID-19.” USA Today, Gannett Satellite Information Network, 10 Apr. 2020, www.usatoday.com/in-depth/news/health/2020/03/05/coronavirus-us-cases-symptoms-travel-deaths-prepare/4904568002/.
9. “How Do SARS and MERS Compare with COVID-19?” Medical News Today, MediLexicon International, www.medicalnewstoday.com/articles/how-do-sars-and-mers-compare-with-covid-19#Coronaviruses-past-and-present.
10. Li, Guoping, et al. “Assessing ACE2 Expression Patterns in Lung Tissues in the Pathogenesis of COVID-19.” Journal of Autoimmunity, 2020, p. 102463., doi:10.1016/j.jaut.2020.102463.
11. @matthewherper, Matthew Herper, et al. “Major Study Finds Steroid Reduces Deaths in Patients with Severe Covid-19.” STAT, 16 June 2020, www.statnews.com/2020/06/16/major-study-finds-common-steroid-reduces-deaths-amon g-patients-with-severe-covid-19/.
12. Paul Webster. The Lancet, Vol. 395, No. 10228. Published: March 21, 2020
13. Poltronieri, Palmiro, et al. “RNA Viruses: RNA Roles in Pathogenesis, Coreplication and Viral Load.” Current Genomics, vol. 16, no. 5, 2015, pp. 327–335., doi:10.2174/1389202916666150707160613.
14. Chow, Nancy, et al. “Preliminary Estimates of the Prevalence of Selected Underlying Health Conditions Among Patients with Coronavirus Disease 2019 — United States, February 12–March 28, 2020.” MMWR. Morbidity and Mortality Weekly Report, vol. 69, no. 13, 2020, pp. 382–386., doi:10.15585/mmwr.mm6913e2.
15. “Q&A On Coronaviruses (COVID-19).” World Health Organization, World Health Organization, www.who.int/news-room/q-a-detail/q-a-coronaviruses#:~:text=symptoms